5.10 Module Summary
Congratulations on completing Module 5! This section gives you the opportunity to review all the material you’ve learned through this module. Take some time to look over the key module figures, which have been duplicated here to remind you of their important content and to summarise the key learning points in this module.
Please then move onto section 5.11 to look through the suggested course reading before taking Module 5 online multiple choice question test.
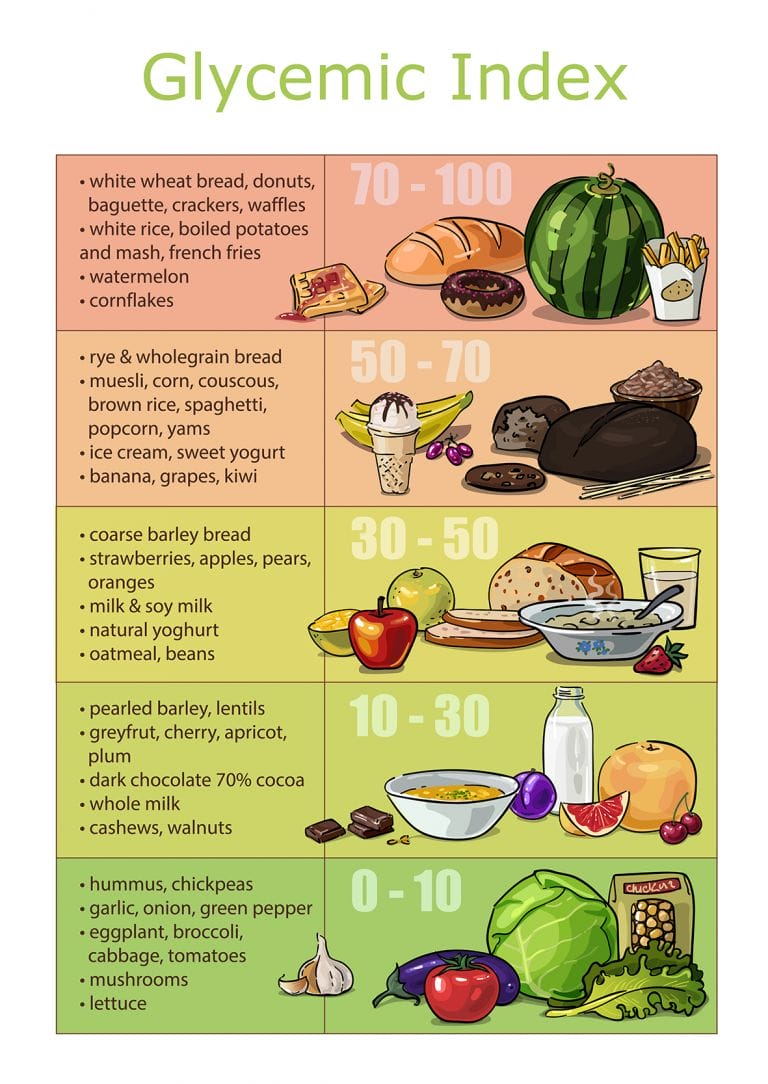


Table 5.3 High and Low FODMAP Foods
| FODMAP | Fructose | Polyols – Sorbitol & Mannitol | Lactose | Fructans & Galactans |
| High FODMAP Food Sources | Vegetables – asparagus, artichokes sugar snap peas
Fruit – apples, pears, watermelon, mango, cherries, figs, tinned fruit in juice, fruit juice, fruit cereal bars, dried fruits Sweeteners – honey, high-fructose corn syrup |
Mannitol – mushrooms, cauliflower,
Fruit – peaches, watermelon Sorbitol – Sweeteners – maltitol, xylitol, and isomalt Fruit – apples, apricots, blackberries, nectarines, peaches, plums, pears Also includes sugar, alcohols and many processed foods
|
Dairy – milk (cow, goat, sheep), yogurt, soft cheeses (ricotta, cottage) | Grains – wheat, rye, bread, pasta, gnocchi, couscous, muesli, wheat bran
Vegetables – garlic, onions, artichokes, inulin, leeks, Fruit – nectarine, peaches, persimmon, watermelon Beans, pulses & legumes including lentils, chickpeas, inulin, FOS Nuts & seeds – cashews, pistachios |
| Lower FODMAP Food Sources | Fruit – citrus, berries, bananas, grapes, honeydew, cantaloupe, kiwifruit, papaya, raspberry, pineapple, blueberry | Sweeteners – maple syrup, sugar, glucose, other artificial sweeteners not ending in “ol”
Fruit – avocado (moderate – ¼ daily) Vegetables – celery (moderate – ½ stalk daily), sweet potato (moderate – ½ cup daily) |
Dairy – lactose-free dairy products, rice milk, soy milk, hard cheeses, coconut milk, butter | Starches – rice, corn, potato, oats, gluten free multigrain breads, quinoa
Vegetables – winter squash, lettuce, spinach, cucumbers, bell peppers, tomato, aubergine, rocket, cabbage (moderate – ¼-½ cup daily), Brussels sprouts (moderate – ¼-½ cup daily), broccoli (moderate – ¼-½ cup daily)
|
Table 6.5 The Reintroduction Phase of the Low FODMAP Diet
| Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday | |
| Week 1. Mannitol and sorbitol (polyols) |
½ cup of mushrooms, 4 dried apricots and monitor symptoms | Monitor symptoms | ½ cup of mushrooms, 4 dried apricots and monitor symptoms | Monitor symptoms | ½ cup of mushrooms, 4 dried apricots and monitor symptoms | Monitor symptoms | Monitor symptoms |
| Week 2. Lactose (disaccharide) |
250 ml of milk or 200g of yogurt and monitor symptoms | Monitor symptoms | 250 ml of milk or 200g of yogurt and monitor symptoms | Monitor symptoms | 250 ml of milk or 200g of yogurt and monitor symptoms | Monitor symptoms | Monitor symptoms |
| Week 3. Fructose (monosaccharide) |
2 tsp of honey and monitor symptoms | Monitor symptoms | 2 tsp of honey and monitor symptoms | Monitor symptoms | 2 tsp of honey and monitor symptoms | Monitor symptoms | Monitor symptoms |
| Week 4. Fructans (oligosaccharide) |
2 slices of wholemeal wheat bread and monitor symptoms | Monitor symptoms | 2 slices of wholemeal wheat bread and monitor symptoms | Monitor symptoms | 2 slices of wholemeal wheat bread and monitor symptoms | Monitor symptoms | Monitor symptoms |
| Week 5. Galactans (oligosaccharide) |
½ cup of lentils or legumes and monitor symptoms | Monitor symptoms | ½ cup of lentils or legumes and monitor symptoms | Monitor symptoms | ½ cup of lentils or legumes and monitor symptoms | Monitor symptoms | Monitor symptoms |
Table 5.7 Advantages and Disadvantages of Different Functional Nutrition Interventions
| Advantages/ Benefits | Disadvantages | |
| Alkaline diets | Increases vegetable intake – improves nutrient and fibre content of diet with associated GI benefits. | Measuring PRAL scores of foods/meals is difficult to do so reality means following list of high alkaline load foods. |
| Reduces processed foods and refine sugar. | Cost of whole foods, meats and vegetables (organic where possible). | |
| Reduces inflammatory markers. | Some people have difficulty digesting grains (IBS). | |
| Vegetarian and vegan diets | Increases vegetable intake – improves nutrient and fibre content of diet with associated GI benefits. | Excluding whole food groups can lead to nutrient deficiencies including Vitamin B12, and zinc. |
| Reduces processed foods and refine sugar. | Vegetarian diets can rely too heavily on cheese/dairy for protein source. | |
| Vegetarian sources of protein are incomplete so careful combination is required to get the levels of amino acids for health. | ||
| Cost of whole foods and vegetables (organic where possible). | ||
| Some people have difficulty digesting grains (IBS). | ||
| May be difficult for some people due to social and family requirements. | ||
| Mediterranean diet | Increasing vegetable intake improves nutrient and fibre content. | Increasing fresh fish intake can be difficult for some people (cost/source) |
| Reducing processed foods and refine sugar. | Still includes grains which may create intolerances/ allergies in some people. | |
| Easy to follow pyramid of food groups. | People who have difficulty digesting fat may struggle consuming 2tbsp olive oil. | |
| Fits into many people’s perception of a healthy diet and all foods easy to source. | Cost of good quality olive oil, meats and vegetables (organic where possible). | |
| Paleo diet | A clean diet without additives, preservatives, or chemicals. | It can get expensive. |
| There are anti-inflammatory benefits from the plant nutrients in fruits, vegetables, oils, nuts, and seeds. | Excludes grains and dairy so difficult to follow and limits certain nutrient choices. | |
| Increase haem iron from increased meat intake | This diet can be difficult for vegetarians, especially since it excludes beans. | |
| Improved satiety — a feeling of fullness between meals – due to the higher intake of protein and fats. | The diet does not specify portions of the allowed foods – may lead to overeating, which could be a problem if you ate a 500g bag of nuts! | |
| Many people lose weight primarily due to the limited food choices. | The diet is higher in protein, and low in carbohydrate, which is the energy source for exercise. | |
| GI Diet | Increasing vegetable intake improves nutrient and fibre content. | Foods with low GI <55 include grains such as rice and pasta, which still contain sugars so spike insulin. Reducing grain, starchy vegetable and fruit intake as per Paleo style diet is therefore often recommended over and above GI diet. |
| Reducing processed foods and refine sugar. | Difficult to remember which are low GI foods – need access to low GI foods table when cooking and eating. | |
| Fits into many people’s perception of a healthy diet and all foods easy to source. | ||
| Fasting/Time Restricted Feeding | Improve sleep and energy by extending natural fasting time overnight. | Fat adaptation can take time so may feel sugar cravings or low energy at beginning of programme. |
| Can still eat same diet and lose weight as body “fat adapts” but for health it’s best to combine with Paleo or anti-inflammatory style foods.
|
Not always suitable for social and family eating patterns. | |
| Don’t need to follow 16:8 diet every day for benefits – can do 2-3 times a week. | ||
| FODMAPs | Relatively immediate relief of IBS symptoms if diet is adhered to. | Very limited food intake – only for short-term use to avoid nutrient deficiencies. |
| Can be complicated for people to follow especially with family and social commitments. | ||
| Reintroduction of foods must be phased to identify any further exclusion. |
- 5.1 Alkaline Diets
- 5.2 Vegetarian & Vegan Diets
- 5.3 Mediterranean Diets
- 5.4 Paleo Diet
- 5.5 Glycaemic Index (GI) Diet
- 5.6 Anti-inflammatory and Auto-immune Diet
- 5.7 Intermittent Fasting & Time Restricted Feeding (TRF)
- 5.8 FODMAP Diet
- 5.9 What Next? Developing Your Own Approach to Functional Nutrition
- 5.10 Module Summary
- 5.11 Recommended Reading & References
- 6.1 What Are Phytonutrients?
- 6.2 Phytonutrient Groups
- 6.3 Evidence For Phytonutrient Anti-Disease Activity
- 6.4 Curcumin
- 6.5 Cannabidiol (CBD) oil
- 6.6 Ashwagandha
- 6.7 Aloe Vera
- 6.8 Supergreens (Alkalising) powders
- 6.9 Gut Supporting Botanicals
- 6.10 Phytonutrient Supplementation
- 6.11 Herbal Laws
- 6.12 Module Summary
- 6.13 Recommended Reading & References
- 7.1 Do We Need Food Supplements?
- 7.2 Nutrient Dietary Reference Values (DRVs)
- 7.3 Vitamins
- 7.4 Minerals
- 7.5 Bioavailability of Food Supplements
- 7.6 Multi-nutrient Formulations
- 7.7 Gut Bacteria
- 7.8 Digestive Enzymes
- 7.9 Saccharomyces boulardii
- 7.10 Essential Fatty Acids
- 7.11 Directional Supplements
- 7.12 Combined Programme
- 7.13 Module Summary
- 7.14 Recommended Reading & References
